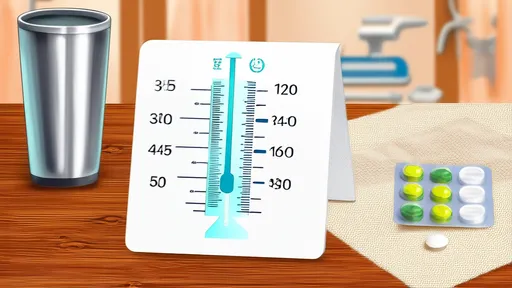
For elderly individuals managing multiple medications, the temperature of drinking water can significantly impact drug efficacy and safety. While most people rarely consider this factor, research suggests that certain medications react differently to hot, warm, or cold water. This often-overlooked detail could mean the difference between optimal treatment outcomes and reduced therapeutic effects—or even potential health risks.
The Science Behind Water Temperature and Medication
Pharmacological studies reveal that water temperature influences how quickly and completely pills dissolve in the digestive system. Cold water may slow dissolution rates for some drugs, particularly those with enteric coatings designed to release medication gradually in the intestines. Conversely, extremely hot liquids (above 60°C) can degrade heat-sensitive compounds in certain antibiotics or thyroid medications. Warmer water generally accelerates absorption for most standard tablets, but exceptions exist—like probiotics requiring cool liquids to preserve live cultures.
Beyond dissolution rates, temperature affects esophageal transit time. Elderly individuals frequently experience decreased esophageal motility, making proper water temperature crucial for preventing pill-induced esophagitis. Lukewarm water proves most effective at facilitating smooth pill passage while minimizing irritation risks—a critical consideration for those taking NSAIDs or bisphosphonates known to cause esophageal damage.
Common Medication Categories and Their Temperature Requirements
Cardiovascular drugs like warfarin and digoxin demonstrate more consistent absorption patterns with room-temperature water. Thyroid medications such as levothyroxine show reduced efficacy when taken with hot beverages due to protein-binding alterations. Surprisingly, many liquid antibiotics (amoxicillin suspensions) maintain stability better when mixed with cool water, while certain antifungal tablets require warm water to activate their special coatings.
Proton pump inhibitors (PPIs) present an interesting case—their delayed-release mechanisms function optimally with slightly warm water that helps the coating dissolve at the correct intestinal location. For elderly patients taking osteoporosis medications like alendronate, cold water increases the risk of esophageal adherence, making tepid water the safer choice. Even common supplements aren't exempt—iron tablets absorb best with vitamin C-rich room-temperature fluids, while fish oil capsules may rupture prematurely in hot liquids.
Practical Implementation Challenges for Seniors
Implementing proper water temperature protocols presents unique difficulties for aging populations. Cognitive impairments may cause forgetfulness about temperature guidelines, while arthritis can make temperature testing physically challenging. Many seniors develop preferences for extremely hot tea or iced water—habits difficult to modify when medication schedules demand different temperatures.
Environmental factors compound these challenges. Nursing home residents often receive medications with whatever temperature water is conveniently available, not necessarily what's pharmacologically ideal. Those living alone may lack reliable thermometers or kettle temperature controls. Economic barriers also exist—some elderly individuals conserve energy by reheating leftover water rather than preparing fresh, properly tempered water for each dose.
Innovative Solutions: Temperature Guidance Tools
Healthcare providers now develop creative methods to communicate temperature requirements. Color-coded medication organizers with integrated temperature indicators (blue for cold, red for warm) help visual learners. Some pharmacies provide "temperature strips" that change color when applied to water containers, offering instant visual feedback. Smart bottle attachments that glow different colors at target temperatures represent emerging high-tech solutions.
For low-tech approaches, caregivers create customized reference charts pairing pill colors with corresponding water temperatures—a system particularly helpful for seniors with limited literacy. Musical mugs that play different tunes at specific temperature ranges engage auditory learners. Occupational therapists sometimes recommend simple analog solutions like floating bath thermometers in drinking glasses—an affordable option with large, easy-to-read displays.
Educational Strategies for Different Learning Styles
Effective education about water temperature requires multimodal approaches. Kinesthetic learners benefit from hands-on demonstrations using temperature-sensitive putty that changes texture at critical thresholds. Visual learners retain information better through infographics showing how hot liquids "melt" medication effectiveness versus cold liquids "freezing" absorption rates.
Auditory teaching methods include rhyming reminders ("Cool for your stool, warm for your arm") or medication-specific jingles. For patients resistant to changing lifelong drinking habits, motivational interviewing techniques help connect proper water temperatures with personal health goals like maintaining independence or reducing hospital visits.
Cultural Considerations in Temperature Guidance
Cultural beverage preferences significantly impact medication adherence. Elderly Asian populations favoring hot tea require tailored education about waiting for beverages to cool before taking certain medications. Mediterranean elders accustomed to icy drinks may need reminders to let water warm slightly for specific drugs. In some cultures, consuming room-temperature liquids contradicts deeply held health beliefs about "warming" or "cooling" foods—requiring culturally sensitive compromise solutions.
Religious practices also intersect with medication timing and preparation. Muslims observing Ramadan may need adjusted temperature guidelines for pre-dawn medications taken without water during fasting hours. Jewish elderly taking medications with hot water on Sabbath face unique preparation challenges under religious law. Sensitivity to these nuances improves compliance.
The Future of Personalized Hydration Guidance
Emerging technologies promise increasingly personalized solutions. Experimental smart pill bottles now sync with smartphone apps to display ideal water temperatures for each scheduled dose. Some prototype systems even dispense pre-tempered water portions when the medication lid opens. Researchers explore edible temperature sensors that change pill coating colors if swallowed with improper-temperature liquids.
Pharmacogenomic advances may eventually allow ultra-personalized temperature recommendations based on individual metabolism rates. Early-stage research examines how genetic variations in drug metabolism enzymes interact with liquid temperatures to affect bioavailability. Such developments could revolutionize geriatric pharmacotherapy within the coming decade.
Until high-tech solutions become widely accessible, simple awareness remains the most powerful tool. Encouraging open conversations between seniors, caregivers, and pharmacists about water temperature habits can prevent countless cases of reduced medication efficacy. Sometimes the smallest adjustments—like waiting five minutes for tea to cool—make the most significant difference in therapeutic outcomes.

By /Aug 15, 2025
By /Aug 15, 2025
By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025
By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025
By /Aug 15, 2025

By /Aug 15, 2025

By /Aug 15, 2025