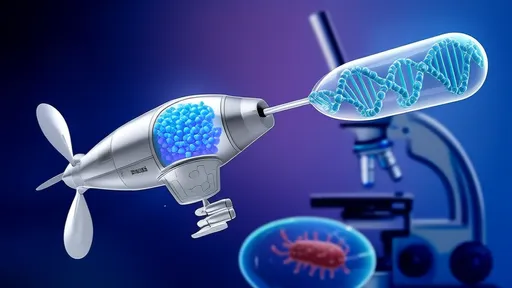
In the relentless battle against antibiotic-resistant bacteria, scientists have turned to nature’s oldest predator—the bacteriophage—and combined it with the precision of CRISPR gene-editing technology. The result? A revolutionary "smart missile" system capable of targeting and eliminating specific bacterial strains with unprecedented accuracy. This breakthrough, dubbed the CRISPR-guided precision antimicrobial system, promises to reshape how we combat infections in an era where traditional antibiotics are increasingly failing.
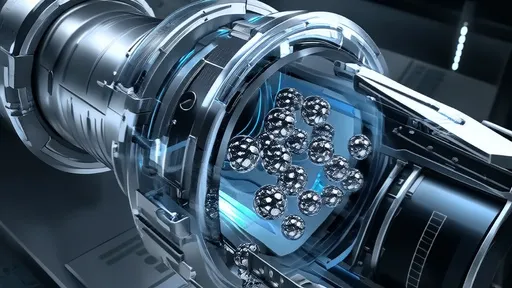
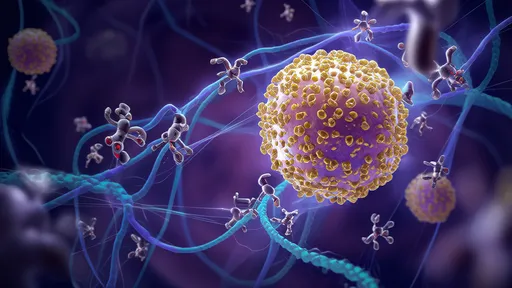
The concept hinges on the natural ability of bacteriophages (or phages) to infect and kill bacteria. Phages are viruses that exclusively target bacterial cells, making them ideal candidates for antimicrobial therapy. However, their natural specificity can be both a strength and a limitation. While phages excel at attacking particular bacterial strains, their narrow host range means they often miss genetically diverse or evolving pathogens. Enter CRISPR—a molecular scalpel that can be programmed to recognize and slice specific DNA sequences. By arming phages with CRISPR systems, researchers have created a hybrid weapon that combines the phage’s infectivity with CRISPR’s programmable precision.
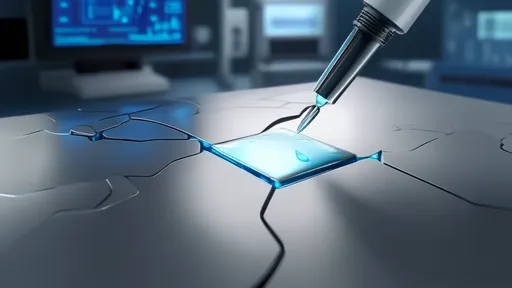
How does this "smart missile" system work in practice? The engineered phages deliver CRISPR components directly into bacterial cells. Once inside, the CRISPR system identifies the target bacterium’s unique genetic signature—whether it’s a virulence gene, antibiotic-resistance marker, or essential survival gene—and cleaves its DNA, effectively inducing lethal cuts. Unlike broad-spectrum antibiotics that indiscriminately wipe out both harmful and beneficial bacteria, this approach leaves the microbiome largely intact. Early experiments demonstrate its efficacy against notorious pathogens like Escherichia coli, Pseudomonas aeruginosa, and even methicillin-resistant Staphylococcus aureus (MRSA).
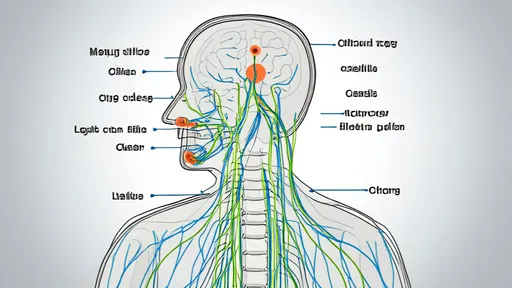
The implications for medicine are profound. Chronic infections, such as those plaguing cystic fibrosis patients or stubborn wound infections, could be selectively eradicated without disrupting commensal bacteria. In agriculture, CRISPR-phage systems might replace prophylactic antibiotics in livestock, reducing the spread of resistance genes. Even environmental applications, like decontaminating water supplies from harmful bacteria, are being explored. Yet challenges remain: ensuring phage delivery to infection sites, preventing bacterial evasion through mutation, and addressing regulatory hurdles for genetically modified therapies.
Critically, this technology also offers a potential solution to the antibiotic resistance crisis. By targeting resistance genes themselves—such as those encoding beta-lactamases or efflux pumps—CRISPR-phages can selectively eliminate resistant strains while sparing susceptible ones. This "resistance-breaking" capability could extend the lifespan of existing antibiotics. Researchers emphasize that phage-CRISPR systems are unlikely to replace antibiotics entirely but could serve as a precision adjunct, especially for recalcitrant infections.
Beyond therapeutics, the platform’s adaptability stands out. The same phage "chassis" can be reprogrammed with different CRISPR guides to target new pathogens as they emerge—a flexibility reminiscent of mRNA vaccine platforms during the COVID-19 pandemic. Startups and academic labs are already racing to optimize delivery methods, from aerosol formulations for lung infections to topical gels for skin wounds. Some envision a future where bespoke phage-CRISPR cocktails are tailored to individual patients’ bacterial profiles.
Ethical and safety discussions accompany this innovation. The deliberate release of genetically modified phages—albeit non-replicating or "disarmed" versions—requires careful scrutiny. Could horizontal gene transfer inadvertently spread CRISPR components to non-target bacteria? Might overuse drive bacteria to evolve counter-defenses? Proponents argue that phages have co-evolved with bacteria for billions of years without catastrophic ecological disruption, suggesting risks may be manageable.
As clinical trials loom, the trajectory seems clear: the marriage of phages and CRISPR represents more than just another antimicrobial tool. It’s a paradigm shift toward intelligent, adaptable therapies that respect microbial ecology while ruthlessly eliminating threats. In a world where 1.27 million deaths annually are attributed to antibiotic resistance (as per WHO 2019 data), such innovation isn’t just welcome—it’s imperative. The era of brute-force antibiotics may be waning; the age of bacterial smart bombs has begun.

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025

By /Aug 5, 2025

By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025
By /Aug 5, 2025